As different hospitals, departments and doctors interact, there exists a potential for mix-ups, and questions of confidentiality to consider. The situation is further complicated by rising global mobility, where greater migration than ever before mixes multiple legislations, languages, notations and insurance systems into our personal health records. Fortunately, there’s an ISO technical committee dedicated to improving the way that our medical information is stored and shared. ISOfocus reached out to discover more about how standardization can improve the flow of information, and patient care.
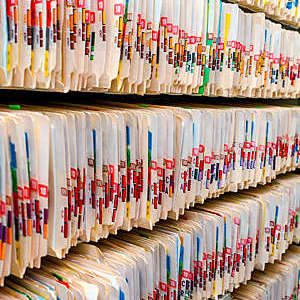
But first, hereʼs what I know about hospitals and patient records. I remember my earliest trip to the hospital with dreamlike clarity. Which is to say, perhaps I misremember details and invent others. (Memories, like all records, are subject to the introduction of error.) However, some things come back in high-fidelity: the bitter smell of cleaning fluids, colour-coded floor lines directing visitors, nurses sorting endless racks of patient cards and smoking.
It seems very different to the hospitals of today; three decades have seen significant advances in almost every area of healthcare. For one thing, the smokers have been kicked out into the cold, but in many hospitals you may still find filing cabinets stuffed to the runners with precious patient data.

Time goes slow
In most other areas that deal with sensitive or important data, we’ve made a choice to leave paper behind. Currencies now exist without the need for banknotes and we’ll happily board an aeroplane without a physical ticket. So why is the move to fully digital patient records taking so long?
It may be because paper works. There is, after all, a foolproof simplicity to getting important things down on pieces of paper and locking them away in a sturdy metal box. (Even the most advanced hospitals are ready to fall back on paper in the event of an electronic systems failure.) But the more likely reason why health records lag behind other personal information systems is the complexity of the transition. In many areas of digitized records and billing, post-digital formats remain much the same, there aren’t really ethical questions to grapple with, and the relationship to the service provider remains mostly unaltered. Going digital with our medical data, or health informatics as it’s referred to by specialists, fundamentally changes the way that we access doctors, and the ways that they can access our most private information. Ultimately, it can even bring new perspectives in assessing conditions and providing care. In other words, a game changer.
Leading a revolution in records
To understand how these changes are being made, ISOfocus spoke to a handful of the experts from ISO/TC 215, the ISO technical committee for health informatics. First on the list is Christian Hay, a man whose 20-year track record in healthcare standardization spans the early development of the barcoding system for drugs that later became known as GS1, as well as significant involvement in developing procedures between pharmaceutical manufacturers and wholesalers, and development of billing procedures for use by health insurers.
To start out, I quiz Christian on the basics. Like, what is the most simple definition of health informatics, and what does it do? “Everything that concerns the use of IT in health” is the pleasingly terse answer to the first part of my question. “It’s basically where technical and medical systems meet.”
Making medicine safer and more effective
 Christian goes deeper with some insights into his own particular area, the pharmacy and medicine business (also the name of the ISO working group that he chairs, ISO/TC 215/WG 6). “Health informatics structures and standardizes information related to medicinal products. In fact, Christian tells me “health informatics applies to every other part of the process from post-marketing surveillance, clinical-decision support, indications and interactions, medical alerts, patient reimbursement and public-health personalized medicine, controlled substances… and more!”
Christian goes deeper with some insights into his own particular area, the pharmacy and medicine business (also the name of the ISO working group that he chairs, ISO/TC 215/WG 6). “Health informatics structures and standardizes information related to medicinal products. In fact, Christian tells me “health informatics applies to every other part of the process from post-marketing surveillance, clinical-decision support, indications and interactions, medical alerts, patient reimbursement and public-health personalized medicine, controlled substances… and more!”
For Christian, the inevitable transition away from paper has “obvious benefits”, but such are only fully realized when “we find globally agreed structures so that information becomes not only digital, but also interoperable between systems”. This is key to opening up exchange between countries, regions and languages. “There is a considerable need for semantics,” Christian continues, which, “for health informatics is partly addressed by ISO/TC 215, as well as by other organizations.”
Connecting through a common language
A slightly different perspective is offered when I connect with Nicholas Oughtibridge. A veteran health standardizer whose experience covers working with the above-mentioned “other organizations” including SNOMED (Systematized Nomenclature of Medicine), BSI (the ISO member for the UK), and the UK NHS, where Nicholas currently leads digital transformation as Head of clinical data architecture. I home in on some of the specifics of his day job. What are the challenges of revolutionizing a tax-funded public-health service? He unhesitatingly replies (like a seasoned standardizer) “bringing together the different parties involved in developing software and managing tensions between different needs, those of business and manufacturers, and those of the health professionals who are providing care”.
It seems logical that with the potential to realize efficiencies and economies of scale, things that work less well are also thrown into relief. There is a huge potential to compound small problems as they are scaled up. By way of proof, Nicholas tells me that “almost 100 % of individual doctors (i.e. general practitioners) are 100 % digital, but there are many hospitals filing significant amounts of paper”. If individual doctors’ offices can reasonably implement their own system, finding things that work for them, part of the challenge of scaling to a national level lies in joining the dots.
Same information, different context
When I ask Michael Glickman, the Chair of ISO/TC 215 and President of Computer Network Architects Inc., to expand on the fundamental notion of health informatics, he tells me that it can also be seen as “the science of computability”. He explains that “informatics allows interoperability, meaning that data collected for one purpose can be safely, effectively and meaningfully used in different settings by computers and individuals”. Across 40 years, Michael has collaborated with more than 600 healthcare organizations, 29 Health Information Exchanges (HIEs) and worked as an active volunteer with numerous non-profit healthcare and information technology standards development organizations and trade associations. His observations are informed by solid experience and, as I reflect further, it opens avenues that seem like a significant shift to me. For example, are we moving toward the possibility of making diagnoses and even treatment decisions based on reliably recorded observations? It strikes me that International Standards to harmonize the way in which we record medical information also create the potential to use patient data for anonymized research. This would of course raise significant questions around consent and confidentiality, and so I ask Michael to explain how these aspects are considered from a standardizing perspective. “Security, privacy and safety are core elements of our work. We have an entire working group (ISO/TC 215/WG 4) dedicated to these subjects and they collaborate with all of our other working groups, as well as dozens of liaison organizations, both within ISO and its affiliates.” It’s reassuring, given the sensitivity of medical data.

Keeping sensitive data safe
Growing concerns around general data use have given rise to legislation like GDPR in the EU (the General Data Protection Regulation 2016/679), and I’m curious to know how legislation such as this impacts the ongoing work of digitizing health records. Nicholas Oughtibridge again: “The point of GDPR is to ensure that people don’t use data in an inappropriate way.” One of the reasons it came into being is that we now handle vast quantities of personal data that we simply didn’t generate before.
Understanding how to treat this appropriately is a challenge that’s better understood when it comes to medical data, where medical professionals recognize that their solemn promise to “do no harm” extends beyond the treatment of physical aspects of patients in their care. Nicholas continues: “Interoperability is still an issue; reliably transferring meaning from one computer or system to another is still the bigger challenge. The benefit of the ISO way is that it encourages broad participation, meaning that ISO standards can adequately represent different national or cultural priorities, while forming a coherent system.”
That’s to be welcomed. Because, whilst I may not be inclined to write about my final visit to a hospital (and, in any case, I hope that it won’t be for a while), I can be confident that the work of ISO/TC 215 is playing a significant part in making it a more joined-up experience. One day, digital records will be the norm, and being asked to fill in the exact same form for the hundredth time will seem just as incongruous as a smoking nurse.